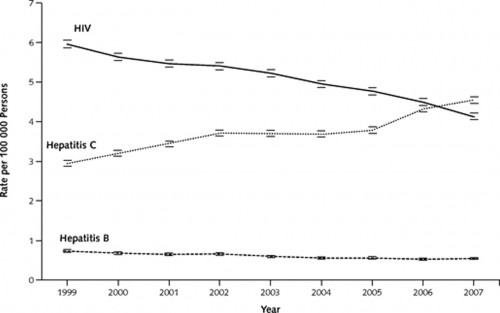
First the bad news:
In summary, even if one cannot easily assign a cause of death among persons with HBV, HCV, or HIV infection, approximately 16 000 deaths among HCV- and HBV-infected persons were registered in 2007, and this figure must represent only a fraction of a larger burden of morbidity and mortality from viral hepatitis.
Our report confirms the rapid growth in viral hepatitis–associated deaths as the baby-boomer generation ages. A recent Institute of Medicine report identified multiple barriers and inadequate public resources to support the prevention, care, and monitoring needed for the public health problem of viral hepatitis. This report focused on low awareness and knowledge of viral hepatitis among the public and health care providers. This factor contributes to inadequate investments in prevention and care services, resulting in missed opportunities to prevent transmission and disease. Recent licensure of point-of-care tests for HCV and several new and more effective therapies for HCV that are in advanced stages of clinical trials increase the opportunities to screen and intervene early and prevent HCV-associated deaths. The Institute of Medicine called for an intensified, coordinated national effort to improve the prevention of new cases and the detection and treatment of discovered persons with this condition.
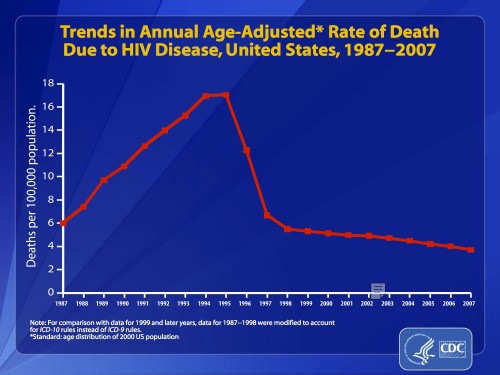
But let’s not miss the good news. If someone had told you 25 years ago that more people in the US would someday die of Hepatitis C than HIV, you would likely have dismissed that person as insane. That’s not because it was crazy to think the number of deaths from Hepatitis C could ever get so high, but because it would have seemed near impossible that the number of deaths from HIV could ever get so low. Here’s a slide of HIV related deaths over a longer period:
This should serve as a testament to what can happen when the health care system commits to a serious program of education, public health, and drug development. It’s an achievement of both the public and private sector. And it should remind us of what we can accomplish when we put our minds to it.
There’s hope for Hepatitis C, too:
In summary, treatments for chronic hepatitis C are evolving at such a rapid pace that in 5 years, interferon-free, oral, direct-acting antiviral regimens may achieve close to 90% cure rates across viral genotypes and regardless of IL-28B allele status. What is currently lacking in this optimistic perspective is a national “find-and-treat” policy aimed at achieving maximum identification of HCV carriers and providing new-generation therapies to a large proportion of those identified cases. The individual and societal benefits of such a strategy are substantial and the costs are in step with other well-established public health measures. The goal to prevent fibrosis progression and cancer evolution in patients with HCV infection is now achievable if our collective will can evolve as rapidly as our pharmacologic skill.