Some readers were less than satisfied with my conclusion of a recent post:
[P]revention can’t play a major role in curbing the rate of growth in health care spending. The rationale for prevention is for health and other economic and social benefits (greater ability to work, enjoy leisure, etc.). [Emphasis added.]
First, note that I did not write “no role,” I wrote “major role.” Second, I was considering the rate of growth. That’s different than shifts in the level of spending. Finally, earlier in the post I noted wide variation across diseases. For some diseases, prevention may have a major impact on health care spending. However, on average the evidence suggests it won’t. These points address Bill Gardner’s concerns, but still may not satisfy everyone.
Maybe this will help: The Robert Wood Johnson Foundation’s Synthesis Project report on Cost Savings and Cost-Effectiveness of Clinical Preventive Care supports exactly what I wrote. First, let’s get some basic concepts straight: cost-saving and cost-effectiveness.
“Cost-saving” and “cost-effective” are distinct terms that are often mistakenly used interchangeably. Preventive care that decreases costs is cost saving. […] If the benefits are sufficiently large compared to the costs, the intervention is “cost-effective” even if it does not save money.
Even for preventive care that is cost-saving, the savings may not be large enough to reverse health care cost trends. Cost savings may slow the growth of health care costs, but be outweighed by other cost growth.
Most preventative care is not cost-saving, but much of it is cost-effective.
The literature on the cost-effectiveness of preventive care is extensive. One registry of cost-effectiveness studies lists more than 500 peer-reviewed articles published on primary or secondary prevention through 2006. Because the literature is so large, this synthesis relies on well-established reviews by others. Reviews conducted by the National Commission on Prevention Priorities (NCPP), the National Business Group on Health (NBGH), and Russell were selected based on several criteria.
Two preventive interventions were found to be cost-saving across all three reviews: childhood immunization and counseling adults on the use of low dose aspirin. Several other preventive measures were found to be favorably cost-effective.
Over thirty types of preventative care were examined. Two were unquestionably cost-saving and 15 others were clearly cost-effective at the $100k/QALY level. (QALY = quality-adjusted life year, a measure of quality and length of life.) I consider this overwhelming evidence that preventative care is not a way to bend the cost curve. It is, however, a way to improve people’s lives. That’s ample reason to invest in prevention. So, I’m not saying don’t prevent disease. I’m saying, it isn’t a solution to our long-term health spending problem, but it is still worth doing.
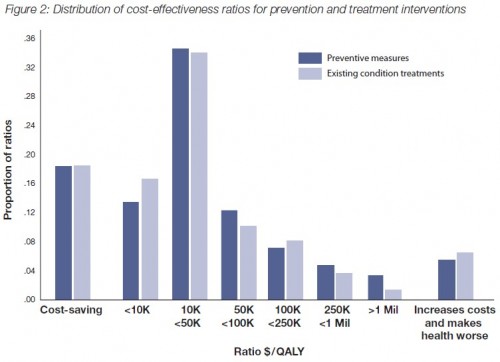
Prevention is important, but it is not obviously more important than treatment of existing conditions. One study (Cohen, et al., NEJM 2008) described in the RWJF report found that “opportunities for efficient investment in health care programs are roughly equal for prevention and treatment.” This is illustrated in the following figure.
All this suggests to me that if one’s interest in prevention is driven by cost-savings or cost-effectiveness, one should focus prevention relatively narrowly. Put another way, and quoting the RWJF report,
Because health care resources are finite, however, it is useful to identify those interventions that deliver the greatest health benefits relative to their incremental costs. In addition, it may be possible to improve intervention cost-effectiveness by targeting higher-risk populations, although identifying high-risk individuals may itself consume substantial resources, depending on how difficult this task is. […]
[P]olicy-makers should consider whether an emphasis on achieving savings from preventive medicine is appropriate. After all, society invests in health care not to save money, but to improve health. A better question to ask — of both preventive medicine and of treatments — is whether current expenditures deliver good value even they do not achieve savings. Focusing on value, rather than on savings, can reduce the risk of overlooking helpful preventive measures. Emphasizing the more realistic goal of good value for all medical care holds the most promise for improving health in a fiscally sustainable manner.