It’s possible the Supreme Court will hand down its decision on the ACA today. I honestly have no idea what they will do, of if we’ll have another week to wait. But some reports put out recently by AHIP are making me nervous. I grant you, they’re not an unbiased player here, but the story is compelling:
In 1993, Washington adopted what then was one of the most extensive health-care reforms ever enacted by a state.
The law promised the grail of near-universal coverage while controlling costs. Waiting periods for pre-existing conditions were effectively abolished and insurers were required to sell policies to anyone who could pay. To attempt to control costs, the law provided for premium caps to be phased in only if competition among insurers failed to moderate increases. It also included mandates that uninsured individuals buy their own policies and that employers pay at least 50 percent of the cost of insuring their workers, and that uninsured individuals buy their own policies.
But the law was not implemented as originally intended, and as Washington residents soon discovered, unless these types of insurance market reforms are paired with an effective requirement for everyone to purchase coverage, serious market disruption is likely, creating real problems for employers, families and individuals.
Critically, key features of Washington’s Health Services Act of 1993 were repealed within 18 months, including provisions that individuals be required to purchase coverage and that employers be required to
offer it to their employees. At the same time, legislators left in force new consumer protection provisions, such as eliminating waiting periods for pre-existing conditions and guaranteeing that an insurance policy would be issued to anyone who could pay. Well-intentioned as these protections were, keeping them in force without strong, effective mechanisms to get everyone in the insurance pool, produced a “death spiral” in the individual market. Higher-risk individuals bought policies that were previously unavailable to them causing premiums to rise, and some healthy people took their chances and dropped their coverage
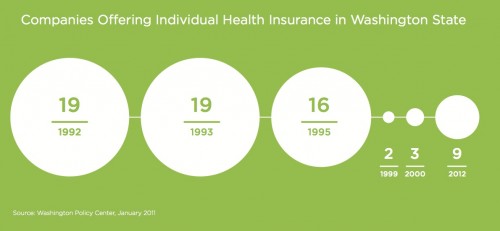
This is the nightmare scenario for the insurance companies. Forced to issue insurance and prohibited from individually rating plans, sick people flood the market. this raises prices, further driving out healthy people. Premiums go up and up and the market enters a death spiral. Insurance companies realize they can’t possible function in this environment, and they leave. Here’s a nice graphic demonstrating the number of insurance companies offering individual policies in WA state over time:
When the law was enacted, there were 19 such companies. Then the individual mandate was struck down. Since the other regulations remained intact, a death spiral started. By 1995, 16 companies remained. By 1999, only 2 companies remained. The rate of uninsured in WA state was 13% in 1993. By 1999, it was 15%.
Years later, other policies have tried to fix this. There are now waiting periods for buying insurance, and government plans for the sickest patients, to remove them from the risk pool. Still, the number of insurance companies offering plans in WA state is less than half that before “reform”.
Lately, there’s been some talk of keeping the “nice” parts of the bill around, while getting rid of the icky mandate. That makes for nice soundbites. It could, however, make for policy that is worse than what we had before. There’s a reason that the mandate, as unpopular as it is, was stuck in the law. There are ways to make the ACA work without a mandate, but all require some sort of legislative action from Congress and the President. That seems unlikely in the near future.