People always seem confused when I simultaneously argue that (1) we spend too much on health care and (2) we have sub-optimal quality. How can that be? The assumption is that there must be a lot of waste; the assumption is that this waste can be easily ferreted out and cut.
The harder thing to accept is that because of our sub-optimal quality, we actually need to spend more on parts of health care. Yes, more.
There’s a new study out in the Annals of Family Medicine that funded in part by the Robert Wood Johnson Foundation. Here are the fine points:
PURPOSE The US Preventives Services Task Force (USPSTF) is authorized by the US government to review and disseminate the scientific evidence for clinical preventive services. The purpose of this study was to evaluate the alignment of Medicare preventive services coverage with the recommendations of the USPSTF before implementation of health reform.
METHODS We recorded all Medicare coverage for preventive services as listed in the Medicare preventive services guide of 2007 (including the 2009 update) for all recommended (A-or B-rated) USPSTF and not recommended (D-rated) guidelines for preventive screening and counseling in adults aged 65 years and older. We analyzed 2 components of preventive care: preventive coordination (risk assessment, patient motivation, and arranging of preventive service) and the preventive service itself. The main outcome measure was the percentage of agreement between USPSTF recommendations and Medicare coverage.
By now you should all know about the USPSTF. They are charged with reviewing the evidence and making recommendations for what preventive services should be offered. Those that receive an A or B rating have significant data behind them and should be performed. This study wanted to see how well Medicare covered such services. Theoretically, insurance such as Medicare should cover such services, as they are proven to provide a benefit, sometimes even paying for themselves. The authors broke out coverage into two parts, coordination (or everything leading up to the service), and the service itself. Here’s what they found:
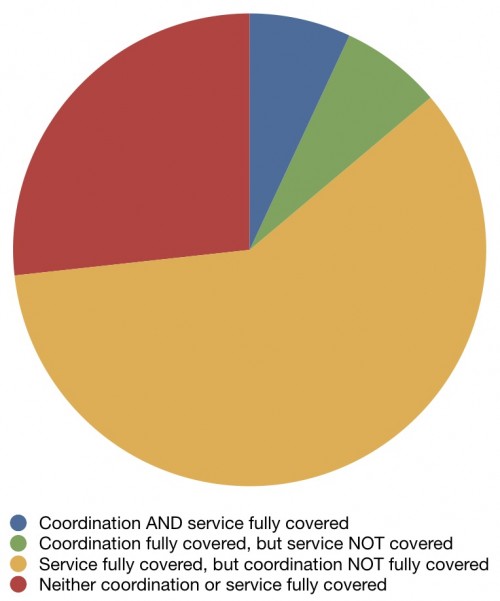
For only 7% of recommendations were both the coordination and service fully covered. For about a quarter of services, neither the coordination nor service were fully covered. For all there rest, coverage was full for one aspect and partial at best for the other.
I’m not saying that insurance should pay for everything, but if we do studies that prove that services have a benefit, then it’s reasonable that those are the things Medicare should cover. Those are the things that will improve our quality. Yes, it will increase the costs of Medicare, but we should pay for these.
The study didn’t stop there, though. They also looked at D rated studies, or those that are not recommended. Here’s a list of screening services that Medicare does cover that the USPSTF does NOT recommend:
- Abdominal aortic aneurysm for women
- Cervical cancer, women >65 y and not at high risk, with adequate screening
- Cervical cancer, women with hysterectomy for benign disease
- Colon cancer aged >85 y
- Coronary heart disease, in low-risk patients
- Ovarian cancer
- Prostate cancer, aged 75 y and older
So we’re confronted with a set of screening recommendations with excellent evidence that aren’t paid for, and a list of screening tests that are recommended against that are paid for. That’s how you wind up with a system that (1) costs too much and (2) has sub-optimal quality. You pay for stuff that doesn’t clearly work and don’t pay for stuff that does.
The problem, however, is that for many Americans, and the politicians who represent them, this doesn’t qualify as waste; it can’t be cut. If we suggest it should be, there are cries of rationing and death panels. But make no mistake about it, this kind of waste is a huge drain on our resources, and until we’re willing to confront it, we will never be able to control health care costs.