Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries, by Arbaje, et al. (Gerontologist, 2008), includes the following figure and passages.
- [O]ne study found that 76% of preventable admissions for congestive heart failure were related to inadequacies in discharge planning, follow-up, social support, or patients’ self-management skills (Vinson et al., 1990). Other studies have found that lack of education (Marcantonio et al., 1999), low SES (Coleman et al., 2004; Weissman, Stern, & Epstein, 1994), and discharge destination (Kind et al., 2007) are associated with early readmission.
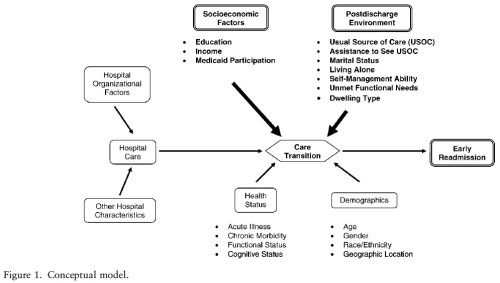
- This study attempts to determine the associations between postdischarge environmental (PDE) and socioeconomic (SES) factors and early readmission to hospitals.
- We conducted a retrospective cohort analysis of community-dwelling respondents to the Medicare Current Beneficiary Survey (MCBS) in 2001 [linked to Medicare claims] who, over 1-year follow-up, were admitted to U.S. acute care hospitals during the period from 2001 to 2002.
- The primary outcome, early readmission, was the occurrence of a nonelective hospital readmission within 60 days of discharge from the index admission.
- Of the 1,351 beneficiaries, 202 (15.0%) experienced an early readmission. After adjustment for demographics, health, and functional status, the odds of early readmission were increased by living alone (odds ratio or OR = 1.50, 95% confidence interval or CI=1.01–2.24), having unmet functional need (OR=1.48, 95% CI=1.04–2.10), lacking self-management skills (OR=1.44, 95% CI= 1.03–2.02), and having limited education (OR = 1.42, 95% CI = 1.01–2.02).
- Results of this study suggest that accommodating PDE and SES factors may be important in improving quality, that is, by assisting in difficult caregiving situations, improving self-management skills, and addressing health literacy. Future studies of interest to institutions and peer review organizations may include the development and evaluation of incentive programs to improve the quality of discharges of older adults, specifically addressing PDE and SES factors. The relationships between hospital organizational factors and early readmission, as shown in Figure 1, also merit further investigation. Specifically, a high degree of centralization (i.e., vertical and horizontal integration) within health systems and the provision of ancillary services important for the care of vulnerable older adults (e.g., case management, palliative care, and transportation) may be associated with early readmission.
Comment: Not all PDE and SES factors are modifiable by hospitals. On the other hand, as the authors suggest, perhaps there are interventions that can assist patients at high risk of readmission due to PDE and SES factors. The main question in my mind is, how much can a hospital do for such patients? Many of these factors are deeply embedded and due to circumstances that have developed over years or decades, if not generations. Where does the hospital’s responsibility end and that of other institutions and culture begin? What is the role of a generally disintegrated health system with a patchwork of coverage programs?