I want to build on Austin’s post from yesterday: a careful read of the literature counters “conventional wisdom” that Medicaid offers abysmal access to its beneficiaries. The studies that Austin considered are retrospective, as studies tend to be. What about the future, with those newly eligible for Medicaid—at least in the 26 states expanding?
The forward-thinking conventional wisdom seems to be along the lines “Well, the expansion will exacerbate the physician shortage. The New York Times reported that, so it’s high time to start freaking out about doctors refusing to see new Medicaid patients.” And pundits have proceeded to do just that. But sometimes research centers do interesting prospective work, too. Consider this report, out of the University of Michigan* and Center for Healthcare Research and Transformation. The researchers surveyed a randomly-generated cohort of primary care physicians in Michigan, and found that generally, the capacity—and intent—to take on new Medicaid patients is there.
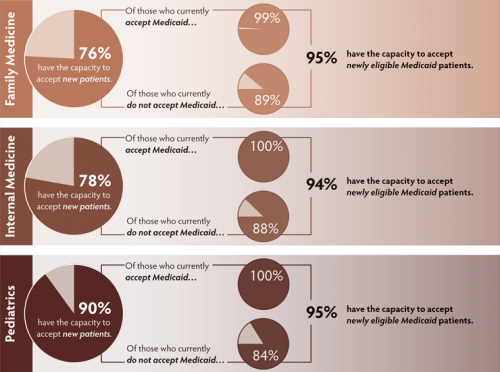
Overall, 81 percent of primary care physicians anticipate expanding their practices to include newly insured patients. Of those physicians, 90 percent of pediatricians; 78 percent of internal medicine practitioners; and 76 percent of family physicians reported that they will have capacity to accept additional patients if the number of Michigan patients with insurance coverage increases in the future.
- Among those physicians who anticipate having capacity for newly insured patients, more than 90 percent expected to have capacity for those newly covered by Medicaid (95 percent of pediatricians; 95 percent of family physicians; and 94 percent of internal medicine practitioners).
- Fifty-five percent of primary care physicians in Michigan reported that they currently accept new Medicaid patients. Almost all of these physicians anticipate having capacity for newly enrolled Medicaid patients in the future (99 percent to 100 percent, depending on the type of primary care).
- Even among physicians who do not currently take new Medicaid patients, most indicated that they would also take newly enrolled Medicaid patients (89 percent of family physicians; 88 percent of general medicine practitioners; and 84 percent of pediatricians).
Or, in charts:
I want to be clear that this survey was specific to Michigan, so mileage may vary. But my home state is probably a pretty solid case study. When it comes to primary care physicians per capita, Michigan is only slightly above the median (the state has 96.8 PCPs per 100,000 residents, compared to national median of 90.5). Michigan’s Medicaid reimbursement rates are nothing to write home about; our Medicaid-to-Medicare fee ratio is below the national average. And still, an overwhelming number of physicians anticipated capacity to serve new patients.
When it comes to health reform, reporters will always be able to find quotes from hand-wringing doctors and placating officials—that doesn’t mean the data will always match up. It’s fair to quibble with this survey; for example, it was conducted during the temporary bump in Medicaid’s primary care reimbursements, which ends after 2014. It needs to be acknowledged that different states will have different experiences; access will suffer most in states with the fewest doctors per capita and lowest Medicaid reimbursement rates. We’ll also observe urban/rural disparities, with access issues exacerbated in less-populous intrastate areas (see this similar survey from Washington state). But the “doctors don’t and won’t accept Medicaid” meme is a radical oversimplification of our best evidence.
*In the interest of full disclosure, the primary author of the CHRT policy brief is a former professor of mine. No grades were helped or harmed in the writing of this blog post.
Adrianna (@onceuponA)