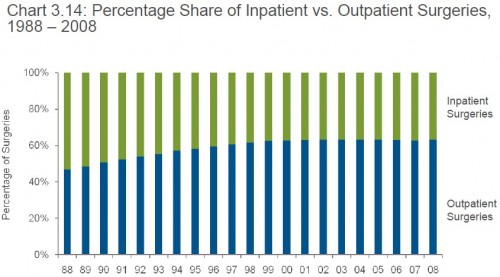
Here’s another interesting figure from the American Hospital Association’s (AHA’s) Trends Affecting Hospitals and Health Systems.
I knew that the majority of surgeries used to be inpatient and that that changed in the 1990s. What I did not appreciate, and this graph shows, is that the inpatient/outpatient breakdown has been constant since 1999. Why did the 1990s trend toward more outpatient surgeries stop completely?
I’m tempted to pin it on the big change in the late 1990s, the backlash against managed care. What’s the mechanism exactly? Is it that insurers had weakened bargaining power with respect to hospitals once they could no longer sell tight networks? Hospitals and the provider system in general had less incentive to keep prices low (outpatient costing less than inpatient) in order to get into insurer networks.
Or does something else explain this? Is it technology? Perhaps the tools that helped move surgeries from inpatient to outpatient stopped improving? If so, why?