I feel like I’ve been spending a lot of time on this topic lately, but it’s one of my issues. I hated residency, and not for the reasons most people think.
Well, it turns out I’m not alone. A new study in JAMA shows that this feeling is pretty pervasive:
Context: Physician distress is common and has been associated with negative effects on patient care. However, factors associated with resident distress and well-being have not been well described at a national level.
Objectives: To measure well-being in a national sample of internal medicine residents and to evaluate relationships with demographics, educational debt, and medical knowledge.
Design, Setting, and Participants: Study of internal medicine residents using data collected on 2008 and 2009 Internal Medicine In-Training Examination (IM-ITE) scores and the 2008 IM-ITE survey. Participants were 16 394 residents, representing 74.1% of all eligible US internal medicine residents in the 2008-2009 academic year. This total included 7743 US medical graduates and 8571 international medical graduates.
Main Outcome Measures: Quality of life (QOL) and symptoms of burnout were assessed, as were year of training, sex, medical school location, educational debt, and IM-ITE score reported as percentage of correct responses.
Big survey of all Internal Medicine residents, looking at quality of life and burnout. Right up my alley.
Let’s start with this: imagine you have worked hard all your life to get amazing grades in order to get into college and then medical school. Then, you spent four more years earning that MD, again competing for limited residency spots. Now, you get to work. But pause and consider what it took to get here:
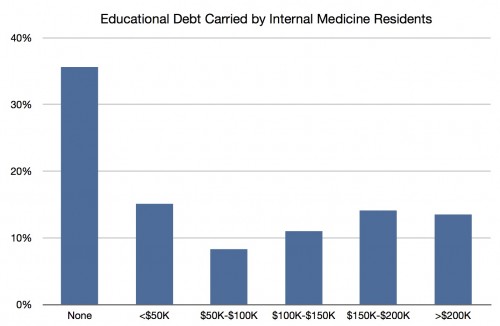
More than 13% of all IM residents had more than $200,000 in education debt. The likelihood of paying this off during residency is slim, so interest accrues massively during those years.
Really, ponder that for a minute. More than $200,000. Do you imagine they are going to be able to buy a house anytime soon? Save for a family? More than a quarter of residents owe more than $150,000 in educational debt. Almost 40% owe more than $100,000.
So right off the bat, that’s going to sting. But then you get the privilige of spending the next three to seven years working for up to 80 hours a week for significantly less money than your education should bring in. The workload is brutal, the system is hierarchical, and it’s genuinely unpleasant. Does this result in a good outcome?
I’m going to drop the snark, because this is absolutely serious. Depersonalization was reported by almost 30% of residents. High levels of emotional exhaustion were reported by more than 45% of residents. Burnout was reported by more than half of residents. That alone should make you pause. This is not a healthy and happy group.
The problem here isn’t just that residents are unhappy and start to lose their empathy, though. It’s that, of all professions, we need them to be empathetic and personal. We need them to care. Yet we have a system that seems completely designed to produce the opposite result.
I still work with residents all the time. I see how unhappy they can be. On more than one occasion, I’ve advised them to consider therapy for depression. People sometimes think I’m intense and unapproachable, but you’d be shocked at how many residents and fellows have cried in my office. I’ve been there; I understand. And, I’m sorry, but I get enraged when physicians “forget” and try to wax nostalgic about a system and profession that seems to value personal martyrdom over having a full life.
Even though they should know better, and we trust them with our lives, physicians are just as likely, if not more likely, to become addicted to drugs. They’re also more likely to have a serious problem before it’s discovered. As I’ve said before, they are more likely to commit suicide than any other profession.
This may sound like whining to some, but I’m not advocating for me. I’ve come out the other side, and I’m OK. But we continue to turn a blind eye to this problem at our own peril.
In this study, almost fifteen percent of residents rated their quality of life “as bad as it can be” or “somewhat bad“. If that doesn’t make you squirm, I don’t know what will.