Chapin White concludes his Health Affairs paper on cost shifting, “My hope is that the dynamic cost-shifting theory is hereby put to rest.”
His work certainly pounds another nail in the coffin.
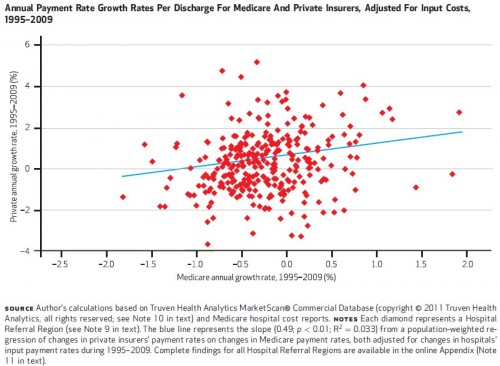
In the two-stage least squares analysis, the estimated elasticity was 0.773, meaning that a 10 percent reduction in the Medicare payment rate was associated with a 7.73 percent reduction in the private rate
The estimate is based on the use of components to changes to Medicare payment rates that are arguably random with respect to private rates, over the 1995-2009 time period. One can’t do much better than that. This is a challenging issue to study.
The paper includes a very nice summary of cost shifting theory. I wish the analysis could have been done at the hospital, rather than the hospital referral region level, but the private price data didn’t allow it. Suffice it to say, despite the high and varied prices hospitals charge, one can’t easily reject the notion that Medicare’s price controls exert downward pressure on them.
All prior cost shifting posts are under the cost shifting tag. There’s also a cost shifting section in the FAQ, which has not been updated in a while.