I’ve often kidded on the square that most of my research is spite based. In other words, something pisses me off, and I go on a mission to prove it’s wrong. My first ever publication was a systematic review showing that conservative therapies didn’t work to help babies with GERD (which Bill Gardner discussed a few weeks ago).
Another pet peeve of mine was the care of failure to thrive. (Pediatric residents all over the country are nodding their heads in agreement right now.) Some babies either don’t gain weight as quickly as we’d like, or they start to lose it. A shockingly large number of them get admitted to the hospital. They get tons of tests and lots of consults, costing thousands of dollars, and the vast majority of them turn out to be functionally normal; they just need to be fed better. What irked me was that so many of them seemed to be admitted over the weekend. Almost all of the tests, and all of the consults, that we’d order would be unavailable then. So it seemed like these babies would just sit. They’d have longer admissions, and they’d cause me a lot of effort and paperwork.
At least, this was my theory. I couldn’t prove it. I tried all the way back in fellowship, but I couldn’t get a good data source. That changed recently.
Some of the people I work with have gotten really good at using the Pediatric Hospital Information System (PHIS). It’s an administrative database that contains inpatient, emergency department, and ambulatory surgery data for forty-three non-profit, tertiary care pediatric hospitals with teaching services in the United States. So I talked my super-awesome fellow (and soon to be junior faculty member) into studying this. The results were published a few months ago, and I’m embarrassed not to have blogged about them before now. “Increased Length of Stay and Costs Associated With Weekend Admissions for Failure to Thrive“*:
OBJECTIVE: To evaluate whether admission day of the week affects the length of stay (LOS) and health care costs for failure to thrive (FTT) admissions.
METHODS: Administrative data were obtained for all children aged <2 years (N = 23 332) with a primary admission diagnosis of FTT from 2003-2011 from 42 freestanding US hospitals. Demographic characteristics, day of admission, LOS, costs per stay, number of discharge diagnoses, primary discharge diagnoses, primary procedure code, number of radiologic and laboratory units billed during admission were obtained for each admission. Linear regression and zero-truncated Poisson regression were used for analysis.
Basically, we looked at length of stay and the cost of admissions for failure to thrive based on day of admission. What did we find? As I suspected, being admitted on the weekend was significantly correlated with a longer LOS and a higher cost. This remained true even when the analysis was restricted to children who turned out to have nothing else wrong, as evidenced by both an admission and discharge diagnoses of failure to thrive. The number of procedures for children admitted on the weekend wasn’t any different than for children admitted on the weekdays – so that didn’t account for the cost difference. Here’s the chart that keeps me warm at night:
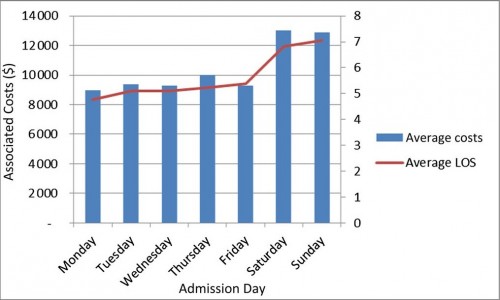
The blue bars (and the left Y axis) are the average cost of a failure to thrive hospitalization by admission day. The red line (and the right Y axis) is the average length of stay by admission day. It would be hard to make a better case that the increased length of stay associated with a weekend admit isn’t the cause of the higher cost.
Our conclusion:
Planned FTT admissions should, when feasible, be scheduled for weekday admission to decrease both health care costs and LOS. Although in some situations, such as an unsafe home environment or a critically ill child, weekend admissions may be necessary, in most cases we believe savings from this simple adjustment could be recouped without a change in health outcomes.
There are so few times in medicine that we can save money with almost no impact on quality. This is one of them. Failure to thrive admissions that include weekend stays are often a waste of money. We should stop doing so many of them.
*This was one of the first publications of a group I spearheaded here at IU, called the Clinical Utilization and Resource Efficiency, or CURE, Group. Our mission is to use data and evidence to find areas of waste in pediatric care. Expect to see more of our work in the future!

