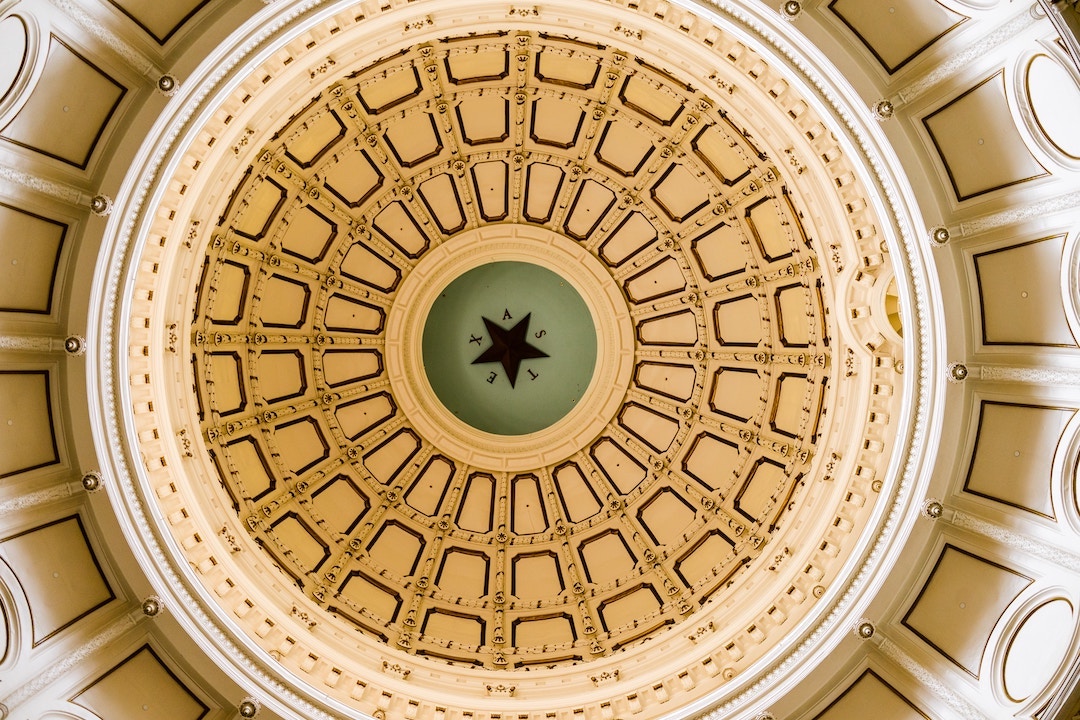
Texas should rethink its approach to phasing out its pandemic-era Medicaid coverage protections; millions of Texans (especially kids) are at risk
Texas recently released its first round of numbers from the “unwinding” of the Medicaid continuous coverage requirement. The state’s approach may be contributing to the coverage losses.