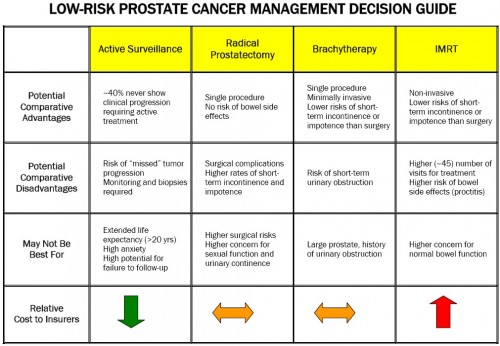
The Institute for Clinical and Economic Review (ICER) has produced a review of the comparative effectiveness and value of treatment options for low-risk prostate cancer. For anyone interested in this topic, it’s worth a look. You might as well be aware of their other reviews too. The low-risk prostate cancer review includes this handy decision guide (pdf):
So, that’s all good. Then, from Health Affairs, there’s this:
The lower cancer detection rates linked to self-referring urologists suggest that financial incentives prompt those urologists to perform prostate biopsies on marginal cases. Thus, self-referral of prostate surgical pathology services leads to increased use and higher Medicare spending, but lower cancer detection rates.
And this:
In a cross-sectional study of prostate cancer patients from 2004 to 2005, we found that regions with lower rates of inappropriate imaging also had lower rates of appropriate imaging. Similarly, regions with higher overall imaging rates tended to have not only higher rates of inappropriate imaging, but also higher rates of appropriate imaging. In fact, men with high-risk prostate cancer were more likely to receive appropriate imaging if they resided in areas with higher rates of inappropriate imaging.
And this:
We found that in the early period of IMRT adoption (2001–03) men with high-risk disease were more likely to receive IMRT, whereas after IMRT’s initial dissemination (2004–07) men with low-risk disease had fairly similar likelihoods of receiving IMRT as men with high-risk disease. This raises concerns about overtreatment, as well as considerable health care costs, because treatment with IMRT costs $15,000–$20,000 more than other standard therapies.
And this:
Forty-two percent of the [direct-to-consumer promotional] pages listed no risks of robotic prostatectomy on the landing page or a page one link away. […]
In a survey of 400 men who had open prostatectomy or robotic prostatectomy, 24 percent of those who had robotic prostatectomy expressed regret with their treatment choice, while only about 15 percent who had open prostatectomy expressed similar regret.
Sigh. Let’s put all that in or near the “bad” category. No surprise here, really. And it clearly is not all bad. Many who received these services (biopsies, imaging, radiation treatment, robotic prostatectomy) benefited or feel they did. Yet, there is tremendous room for efficiency gain in our health system, corresponding to appropriate application of comparative effectiveness evidence and shared decision making. Naturally, many well-meaning policy initiatives toward this end might cause too abrupt a disruption and loss of income for certain types of providers, which is the source of resistance to them. So, why not pay for efficiency and use of evidence and consumer-involvement and penalize in cases of lack of application of them? It may cost something (or save less than blunt cuts, which are politically challenged anyway), but at least we’d be getting something for our money.
So, what about “ugly?” Look no further than the Wall Street Journal. Bill Gardner provides a counterpoint.