This post is jointly authored by Austin Frakt and Yevgeniy Feyman.
Like everything in health care, network adequacy is complicated, with numerous measures and differing regulations by program. This post offers a flavor and a bit of organization of that complexity, based on some of our recent reading.
Medicare Advantage
When is network adequacy assessed? CMS is only certain to assess a plan’s network upon application for a new contract or expansion of a contract’s service area. At its discretion, CMS may review networks at other times, for instance when a plan terminates a contract with a provider, when it changes ownership, or when there are network access complaints or plan-identified network deficiencies.
What types of entities are assessed for adequacy? There are different network adequacy standards for each of 27 practitioner specialty types (e.g., primary care, cardiology, urology) and 23 facility types (e.g., acute inpatient hospitals, outpatient dialysis, mammography).
Are all markets treated equivalently? No. CMS places each county into one of five categories: Large Metro, Metro, Micro, Rural, or CEAC (Counties with Extreme Access Considerations). Within each practitioner and facility type, there are different network adequacy standards by county type. These can change from year-to-year as well.
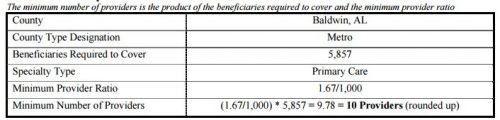
How is network adequacy measured? The gist is that each plan must contract with a specified number of providers of each type. Moreover, 90% of beneficiaries in the county must live within specified travel distance and travel time from at least one provider of each type. To calculate the minimum number of providers, each county receives a population of beneficiaries (termed “beneficiaries required to cover” in the table below) that is equal to the 95th percentile of penetration in all plans in its county type, multiplied by the total number of beneficiaries in the county. That’s a mouthful, but roughly speaking it means that CMS makes sure that each plan can serve a number of beneficiaries larger than it is ever likely to enroll.
This is rather abstract. How about a concrete example? Sure! The following tables should help. The first illustrates the calculation of the number of primary care providers a plan in Baldwin, AL must contract with (10) for 5,857 beneficiaries.
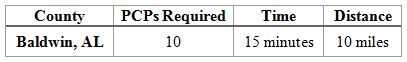
The next table shows that in Baldwin, AL, at least one primary care provider must be within 10 miles and 15 minutes of travel time for 90% of beneficiaries in the county. Additionally, a PCP who is not within the time and distance requirements of at least one beneficiary, will not count towards the minimum number of providers required. Moreover, because at least 90% of beneficiaries must be within the time and distance requirements, a plan may have to contract with more than the minimum number of providers required to meet these requirements.
Where can I learn more? Here are some potentially helpful links:
- Most of the foregoing can be found in this CMS guidance document.
- Additional details on how time and distance to providers are calculated can be found in this memo.
- Here is the most recent file that specifies year-specialty-county type network adequacy regulations.
Marketplaces
The following is for federally facilitated marketplaces, but concludes with a comment about state facilitated ones.
When is network adequacy assessed? As best we can tell, network adequacy is assessed for each plan every year.
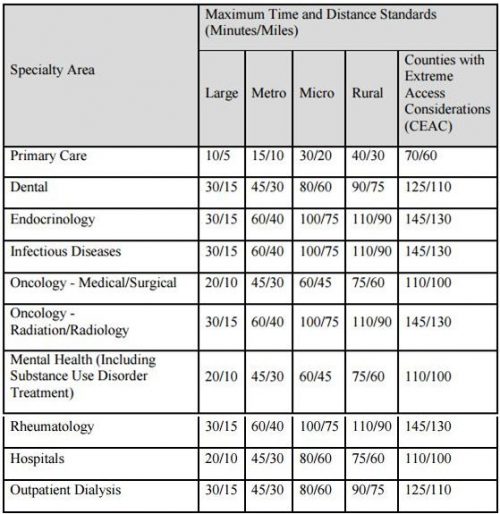
What types of entities are assessed for adequacy? CMS focuses on a subset of specialist areas and facility types that have been associated with network adequacy problems in the past: hospital systems, dental providers (if applicable), endocrinology, infectious disease, mental health, oncology, outpatient dialysis, primary care, and rheumatology. That other specialists and facility types are not necessarily scrutinized is one limitation of the approach.
Are all markets treated equivalently? No. CMS places each county into the same categories used for MA plans’ network adequacy: Large Metro, Metro, Micro, Rural, or CEAC (Counties with Extreme Access Considerations). Within each practitioner and facility type, there are different network adequacy standards by county type. Presumably, these can change from year-to-year as well.
How is network adequacy measured? The approach is similar to that for MA plans: 90% of enrollees must have access to at least one provider/facility type within specified travel distances and travel times. A key difference is that there does not appear to be a minimum number of each provider type every plan must contract with. It’s reasonable to hypothesize, therefore, that marketplace plans would have much more narrow networks than MA plans, but no direct comparison exists, to our knowledge.
This is rather abstract. How about a concrete example? The table below lists the time and distance standards by county and provider type.
Where can I learn more? Here are some potentially helpful links:
- Most of the foregoing can be found in this CMS letter to issuers.
- Here is a link to the RWJF network adequacy and travel standards dataset
- States also have network adequacy statutes and regulations. Historically, most applied to HMOs. Details here and here.
UPDATE:
For how states can make up for lack of 2018 review & other problems in marketplace rule see: https://t.co/R3D6wMryvH (3/3)
— Claire McAndrew (@claire_mcandrew) August 30, 2017