This is a TIE-U post associated with Karoline Mortensen’s Introduction to Health Systems (UMD’s HLSA 601, Fall 2012). For other posts in this series, see the course intro.
In Primary Care — Will It Survive (NEJM, 2006), Thomas Bodenheimer wrote,
The hospitalization rates for diagnoses that could be addressed in ambulatory care settings are higher in geographic areas where access to primary care physicians is more limited. States with a higher ratio of generalist to population have lower per-beneficiary Medicare expenditures and higher scores on 24 common performance measures than states with fewer generalist physicians and more specialists per capita.
This reminded me of two other papers. The first is Medicare Spending, The Physician Workforce, And Beneficiaries’ Quality Of Care, by Katherine Baicker and Amitabh Chandra who wrote,
This suggests that specialists are clustered in areas where costly intensive care crowds out high-quality care and that one mechanism for this is a lesser presence of general practitioners. Encouraging greater access to general practitioners, or involving specialists in the provision of effective care, could improve the overall quality of care received by elderly Americans.
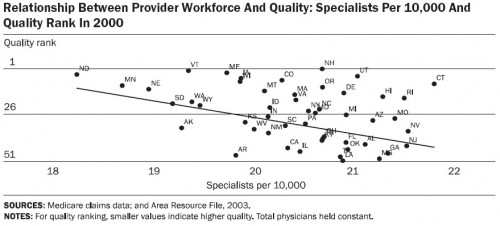
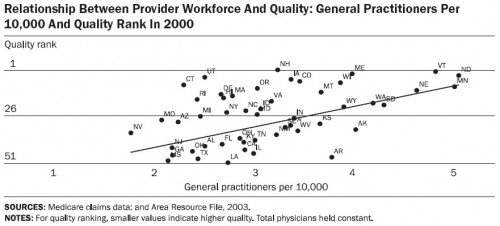
Their charts and tables tell the story. Below are four that support both quotes above. First, let’s consider how state quality rank relates to physician workforce composition. And by quality rank I (they) mean the average of the ranks for the 24 quality measures developed by the Medicare Quality Improvement Organization. The more specialists per capita, the lower a state’s quality rank. (Note: for all charts, total physicians per capita is held constant.)
But the more general practitioners per capita, the higher the state’s quality rank.
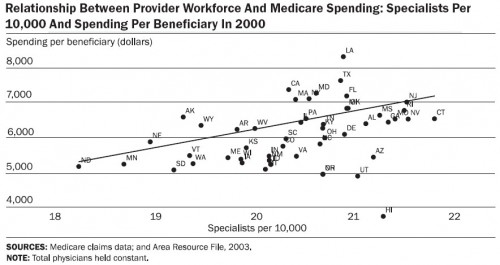
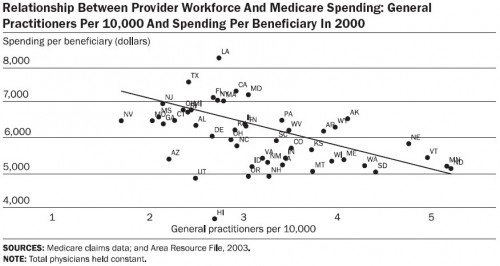
What about spending? Well, specialists cost a lot more than general practitioners. Here are the charts, first specialists and then general practitioners:
If these charts look familiar, you may recall I wrote about them before.
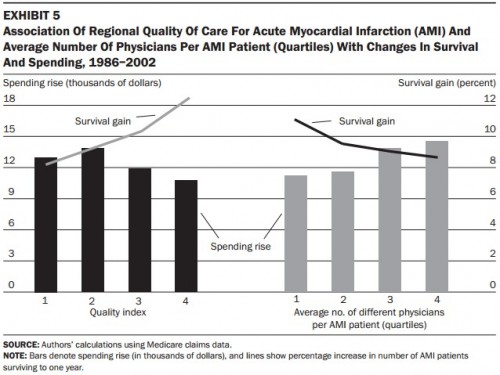
The other paper that came to mind is by Jonathan Skinner, Douglas Staiger, and Elliott Fisher and about which I wrote once before. It includes a terrific, if busy, chart that shows region-level relationships between survival gains for Medicare patients with acute myocardial infarction (AMI or heart attacks) and aspects of the health systems in which they received care.
I explained this chart in detail before, so I won’t here. Click through if you need help getting oriented. I concluded,
The take-away is that the increases in productive efficiency (health gains per spending increase) of regions varies according to how regions deliver care. (This is almost tautological.) Regions that do the basic, low-tech things well (like consistently giving aspirin and beta-blockers to AMI patients at discharge) and offer better coordinated care (e.g., by having fewer physicians treating an AMI episode) are more productively efficient.
Over-use of specialty care and under-use of primary care certainly seems like a mechanism by which we achieve higher cost and worse outcomes. I assert that this is not intuitive to a typical consumer who lacks a high-level view of the health system. Almost nobody who isn’t well versed in health care would say that more access to specialists is a bad thing. Does this reflect a communication failure by health system researchers?