Is it only Thursday? Well, that means Aaron and I are still at it on Ezra Klein’s blog. Here’s a cross-post of my latest. The original is here.
I’m not a physician, but I’ll go out on a limb and guess that operating with a hatchet instead of a scalpel would run counter to best practice.
Likewise, taking a meat ax to Medicare is also not a sound strategy. Yet, that’s what is often suggested, figuratively speaking, in the name of health reform. The temptation is to solve Medicare’s spending problem by cutting payments to providers either outright or by shifting them to beneficiaries, as Republicans in Congress have voted to do. A slight variation is to reduce regional variation in Medicare spending by cutting (or reducing the growth in) provider payments in high spending areas and increasing them in low spending areas.
However, none of these approaches are health reform we should welcome if they don’t improve health. Would they? No.
In a new paper in Health Services Research, Jack Hadley, Timothy Waidmann, Stephen Zuckerman, and Robert Berenson explain why. (The paper is gated, but you’ll find more at the Robert Wood Johnson Foundation). In a beneficiary-level analysis using survey data linked to Medicare administrative records, they found that higher medical spending predicts better health.
To the extent that our results indicate that on average, across the entire range of medical spending and health conditions, the relationship between medical spending and health is positive, then across-the-board reductions in or limits on Medicare spending may result in poorer health for some Medicare beneficiaries. Moreover, because the variation in medical spending in our analyses was driven by variations in practice patterns across geographic areas […] then targeting Medicare spending reductions on geographic areas with high average Medicare costs per beneficiary would also appear to be unwarranted.
In other words, according to their findings, cutting Medicare reimbursements to providers would harm health, even in areas with above average spending. A hatchet is the wrong tool.
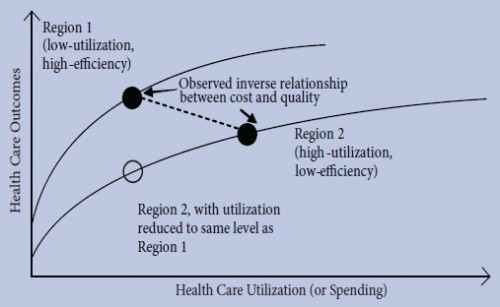
Yet, there is other work that suggests high spending areas have worse health outcomes. However, paradoxically, cutting spending in that case is the wrong thing to do too. The reason is explained with a figure by Jill Bernstein, James Reschovsky, and Chapin White in a National Institute for Health Reform paper (ungated PDF), reproduced below. (The figure was adapted from an earlier one published by Jonathan Skinner, Douglas Staiger, and Elliott Fisher in Health Affairs (ungated PDF).)
The figure depicts the health system performance of two regions. Region 1 has low utilization (low spending) and high efficiency (i.e., very little low effectiveness care is provided). Region 2 has high utilization (high spending) and low efficiency (i.e., a lot of care that is not very effective is provided). The two regions have different health outcomes production functions. That is, the relationship between health care utilization (spending) and outcomes is different in the two regions, as shown by the two lines in the figure.
Spending is higher in region 2 than 1 but outcomes are worse (black dots). Based on this, we might conclude that higher spending produces worse health outcomes, and that we should therefore cut spending in region 2. However, doing that would shift region 2 down its health production function to the empty circle in the figure. At that point, region 2′s outcomes are even worse than they were to begin with. In other words, cutting reimbursements does reduce utilization, but it does so in a way that is harmful to health.
The mistake here is that high spending may be correlated with poor outcomes, but it does not cause poor outcomes. And, if the results ofHadley, Waidmann, Zuckerman, and Berenson are correct, higher spending may even improve outcomes. (That’s not inconsistent with the figure above. It’s just a different choice of spending in the two regions so that region 2’s dot is higher than region 1’s.)
So, if we can’t just whack spending and expect better outcomes, what can we do? The answer must lie in more nuanced reforms to payment policy, towards a system that rewards the good performance we seek. That is, we need a scalpel, not a hatchet. That’s an obvious conclusion, neither helpful nor controversial.
Slightly less obvious – if you don’t know the research – is that there isno evidence that beneficiaries know how to select good performance even when they’re required to pay for it on their own. When they economize, they cut both helpful, necessary care and wasteful, useless treatment in about equal amounts. To continue the metaphor, beneficiaries don’t know how to use scalpels. This is the fatal flaw in the Republican plan for Medicare.
Potential solutions to the spending conundrum are embedded in current law. They include the accountable care organization model, other pay-for-performance incentives, comparative effectiveness-driven practice, and whatever the Independent Payment Advisory Board dreams up.
Does this sound like I just invoked a bit of wishful thinking? Well, I confess, I have! (More on exactly that later.) Though not all of these ideas are completely untested, they are not fully tested and proven to solve our health spending problem while improving health on a national scale. Yet, they are worthwhile experiments; they are scalpels, or can be. Importantly, they focus on health, not just on spending. Any health reform that only focuses on the latter misses the point.