This is a TIE-U post associated with Jonathan Oberlander’s Political Dynamics and Policy Dilemmas (UNC’s HPM 757, Fall 2011). For other posts in this series, see the course intro.
In a 2005 Health Affairs article, a team from RAND, Hillestad et al., [1] estimate massive savings from widespread adoption of electronic medical record (EMR) systems.
EMR implementation and networking could eventually save more than $81 billion annually—by improving health care efficiency and safety—and that HIT-enabled prevention and management of chronic disease could eventually double those savings while increasing health and other social benefits.
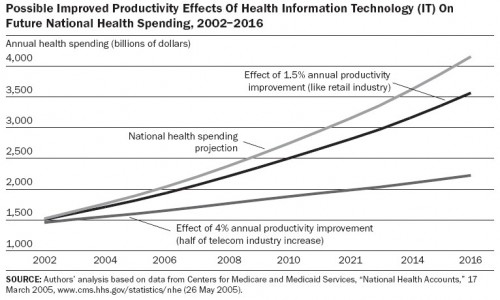
Productivity in the health sector is relatively low and raising it could go a long way toward addressing the rapidly growing US health budget, as the authors illustrate.
The authors advise caution in interpreting the estimated effects of EMR adoption, stressing they are reporting “potential savings,” by which they mean those “assuming that interconnected and interoperable EMR systems are adopted widely and used effectively.”
I’ll add my own word of caution: the study is not based on anything like a comparison (randomized or otherwise) between systems that have and have not implemented EMRs of the type assumed for analysis. This is, as is essentially admitted by the authors, a thought experiment about a world not like the one in which we currently live. (There’s nothing wrong with that. But it does threaten the generality of the findings.)
Here’s another cautionary note, this time from the CBO:
[T]he RAND study was based solely on empirical studies from the literature that found positive effects for the implementation of health IT systems; it excluded studies of health IT that failed to find favorable results.
In 2006, also in Health Affiars, Jaan Siderov [2] throws some more cold water on the idea that EMRs can produce the kind of productivity increases and savings Hillestad et al. suggest might be possible. Citing literature, he writes that
- “EHR[s] increased documentation time among physicians by approximately 17 percent, while computerized provider order entry (CPOE) increased it by 98 percent.”
- “EHR[s] can ‘auto-populate’ or scour the record to justify a greater intensity of service. Accordingly, ‘increased coding levels’ account for the return on investment.”
- “EHR decision support has no effect on adherence to primary care guidelines for asthma or angina management; it leads to ‘variable’ and ‘limited’ adherence to diabetes and coronary artery disease reminders; it has no effect on evidence-based interventions for heart disease and heart failure; it causes no change in the care of patients with depression; it leads to ‘unwieldy’ tracking and monitoring of preventive health and chronic illness; and it has no impact on diabetic glucose control.”
- “75 percent of physician respondents admitted ignoring reminder icons, and more than half seldom or never acted on the information.”
- “‘Profit center’ laboratory or radiology departmentswill not necessarilywelcome EHR-based interventions that lead to fewer tests and less revenue.”
- “More lives saved will come at a heavy price.”
Siderov cites research in support of these statements. I’ve omitted them because there is an ungated version of Siderov’s paper available. However, all are just as plausible, if not more so, than the assumptions made by Hillestad et al. They suggest to me that much more than effective use of widespread, interoperable EMRs (or EHRs)* is necessary to achieve dramatic reductions in health spending and improvements in health. This sentiment is echoed by others as well (e.g. DesRoches et al. [3] in Health Affairs, 2010).
A lot of what must be done has nothing to do with information technology at all. That’s not to say health IT can’t play a role. It can. It just isn’t so clear that it will be the cause of whatever success we achieve (if any).
* I have glossed over the differences between EMRs and EHRs. One of the papers discussed uses the former, the other the latter. Do you think those distinctions matter to what they or I have written? If so, let me know.
References
[1] Richard Hillestad, James Bigelow, Anthony Bower, Federico Girosi, Robin Meili, Richard Scoville, and Roger Taylor. Economics Of Health Information Technology: Can Electronic Medical Record Systems Transform Health Care? Potential Health Benefits, Savings, And Costs. Health Aff. September 2005. 24:51103-1117; doi:10.1377/hlthaff.24.5.1103
[2] Jaan Sidorov. It Ain’t Necessarily So: The Electronic Health Record And The Unlikely Prospect Of Reducing Health Care Costs. Health Aff. July 2006 25:41079-1085; doi:10.1377/hlthaff.25.4.1079
[3] Catherine M. DesRoches, Eric G. Campbell, Christine Vogeli, Jie Zheng, Sowmya R. Rao, Alexandra E. Shields, Karen Donelan, Sara Rosenbaum, Steffanie J. Bristol, and Ashish K. Jha. Electronic Health Records’ Limited Successes Suggest More Targeted Uses. Health Aff. April 2010 29:4639-646; doi:10.1377/hlthaff.2009.1086