Over the last several years, Gretchen Jacobson, Anthony Damico, Jennifer Huang, and Tricia Neuman have posted four papers on the Medicare Advantage (star) quality ratings. They’re relatively quick reads and chock full of facts and charts. Below are a few excerpts of details I want to keep in mind or thought might interest readers. Though the post is long, it is by no means a complete summary of the content of the papers. If you’re in a hurry, you might at least want to scroll down to see the charts.
Background:
- “Medicare Advantage plans are rated on a 1 to 5 star scale, with 1 star representing poor performance, 3 stars representing average performance, and 5 stars representing excellent performance. The quality scores [] are based on 53 performance measures that are derived from plan and beneficiary information collected in three surveys – HEDIS® [Healthcare Effectiveness Data and Information Set], CAHPS® [Consumer Assessment of Healthcare Providers and Systems], and HOS [Health Outcomes Survey] – and administrative data [on plan quality and member satisfaction]. For example, the performance measures include whether the plans’ enrollees received the appropriate screening tests, the number of complaints CMS received about the plan, and how enrollees rated the communication skills of the plans’ physicians. CMS assigns quality ratings at the contract level, rather than for each individual plan. This means that every Medicare Advantage plan covered under the same contract receives the same quality rating (and most contracts cover multiple plans).”
- “[Administrative data from CMS that informs the quality ratings] includes information about member satisfaction and disenrollment, as well as plans’ appeals processes, audit results, and customer service. CMS groups the individual quality measures into five domains: (1) staying healthy: screenings, tests, and vaccines; (2) managing chronic conditions; (3) ratings of health plan responsiveness and care; (4) health plan member complaints, appeals, and choosing to leave the health plan; and (5) customer service.”
- “The individual measures and the scores comprising the summary score are adjusted for skewness, to avoid a clustering of scores at either the high or low end. The individual measures are also adjusted for patient characteristics, to make the survey results more representative of all beneficiaries enrolled in Medicare Advantage.”
- “The CAHPS® responses, for example, are generally adjusted for age, education, mental and physical health status, eligibility for Medicaid, eligibility for Medicare Part D low-income subsidies, state of residence, and whether the survey was completed by the enrollee or a proxy. The composite score also takes into account whether contracts have demonstrated both high and stable quality ratings across all measures, relative to other contracts.”
- “CMS does not publish quality ratings for a plan if it is missing too much data to calculate a score for a given measure or component of the summary score. Relatively newer plans are less likely than older plans to have ratings because of missing data. All plans offered for the first time in 2009 or 2010 do not have quality ratings for the 2010 plan year, because the plans would be missing data from the earliest survey, HEDIS®, which collected data from January to December 2008. Very few plans offered for the first time in 2008 were rated for 2010. Plans with relatively low enrollment are also more likely to be missing data because contracts with less than 1,000 enrollees are not required to report HEDIS® data to CMS. Private Fee-For-Service (PFFS) plans are more likely than other plan types to be missing data, and therefore not have quality ratings, because they are not required to report HEDIS® data until 2010, and many PFFS plans are relatively new.”
- “Medicare Advantage organizations report the quality data at the contract level.”
- “More than half (59 percent) of 2010 Medicare Advantage plans received quality ratings; these plans account for 85 percent of all beneficiaries in Medicare Advantage plans, based on 2009 enrollment.”
- “[I]t is not possible for all contracts to significantly improve their quality rating in the same year because performance measures are scored on a relative scale (or “curve”) for each measure.”
Ratings are positively correlated with:
- Not-for-profit status
- Duration of plan experience in Medicare
- Being an HMO (as opposed to a PFFS and PPO plan)
- Operating in an urban area
- County-level Medicare Advantage penetration (proportion of beneficiaries in MA)
- Median household income
- Number of plans in an area
Provisions of the ACA:
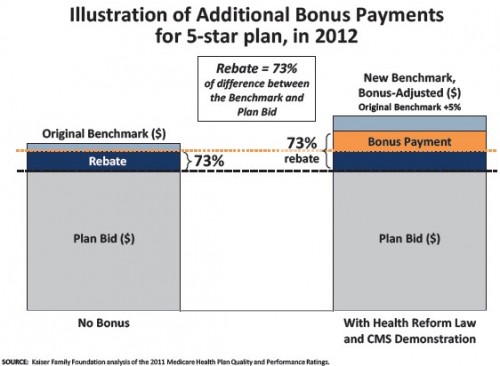
- “[P]lans with higher quality ratings will receive higher rebates: a 70 percent rebate for plans receiving 4.5 or 5 stars; a 60 percent rebate for plans receiving 3.5 or 4 stars; and a 50 percent rebate for plans receiving 3 stars or fewer. Plans with 4 or more stars will also receive bonus payments (i.e., additional amounts added to the plan’s benchmark), and in certain counties, they will receive double bonuses.”
- “[T]he health reform law required bonuses to be doubled for plans that are offered in counties with all the following characteristics: 1) lower than average Medicare fee-for-service costs, 2) a Medicare Advantage penetration rate of 25 percent or more as of December 2009, and 3) a designated urban floor benchmark in 2004. In 2012, Medicare Advantage plans in 210 counties will qualify for double bonus payments”
- “In 2012, all small or low-enrollment plans will receive quality bonuses, and rebates of 70 percent of the difference between the bid and the benchmark; the Secretary of Health and Human Services is required to establish a method for computing quality ratings for small plans for 2013 and subsequent years.”
- “All new plans will receive quality bonuses (1.5 percent in 2012, 2.5 percent in 2013, and 3.5 percent in 2014) and rebates of 65 percent of the difference between the bid and benchmark in 2012 and subsequent years. New plans are defined as those offered by organizations that did not have a Medicare Advantage contract in the previous three years.”
- “CMS has also stated that, since plans have no opportunity to change their ratings for 2012, and little opportunity to change their ratings for 2013, the agency may modify and upwardly adjust the quality rating summary scores for the purpose of making bonus payments in 2012 and 2013 to allow plans some time to transition.”
- “Most Medicare Advantage contracts (91%) will receive a bonus payment in 2012 because they received 3 or more stars, or were not rated; the remaining 9 percent of contracts will not receive bonus payments because they received 2 or 2.5 stars.”
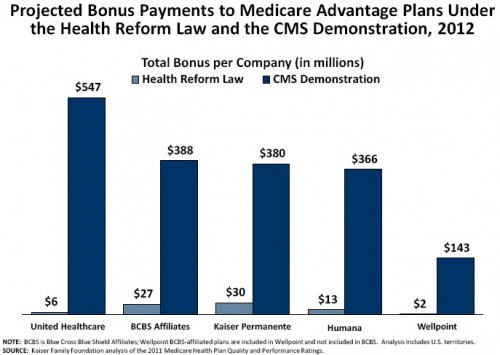
- “About one-third of the total bonus payments ($1.1 billion) are projected to go to plans rated as above average or better (4 or more stars), and two-thirds ($2.0 billion) are projected to go to plans rated as average (3 or 3.5 stars) and plans that were not rated.”
Modification by of ACA provisions by CMS demonstration authority:
- “First, all ratings would be based on the contracts’ overall scores, rather than the summary scores. [I don’t understand what this means.] Second, bonus payments would be provided to contracts that are rated as average performers (3 or 3.5 stars), in addition to those that receive 4 or more stars. Third, contracts that receive 4 or more stars would receive higher bonus payments than those authorized under the health reform law. Fourth, contracts that receive 5 stars would receive higher bonus payments than the 4 and 4.5 star contracts and would not be subject to the bonus cap; the cap would still apply to all other contracts. Lastly, bonuses for contracts that receive 5 stars would be applied to the blended benchmark, rather than just the new benchmark, providing the 5 star plans the full bonus amount before the changes are fully phased‐in. Bonuses for all other contracts would be applied to only the new benchmark.”
- “The additional bonuses provided under the demonstration in 2012 are expected to amount to about half of the reduction in Medicare Advantage plan payments ($6 billion) included in the health reform law for 2012.”
Prior TIE coverage of Medicare Advantage quality bonuses can be found in this Google Custom Search.